Mpox, formerly known as monkeypox, has emerged as a topic of significant concern in recent years, particularly following the global health alerts around its spread. Despite this, it is essential to recognize that mpox is not a new disease to India. Historically, India has seen sporadic cases, and understanding how mpox spreads, its risk factors, and its differences from airborne diseases like COVID-19 is crucial for public awareness and health management.
What is Mpox?
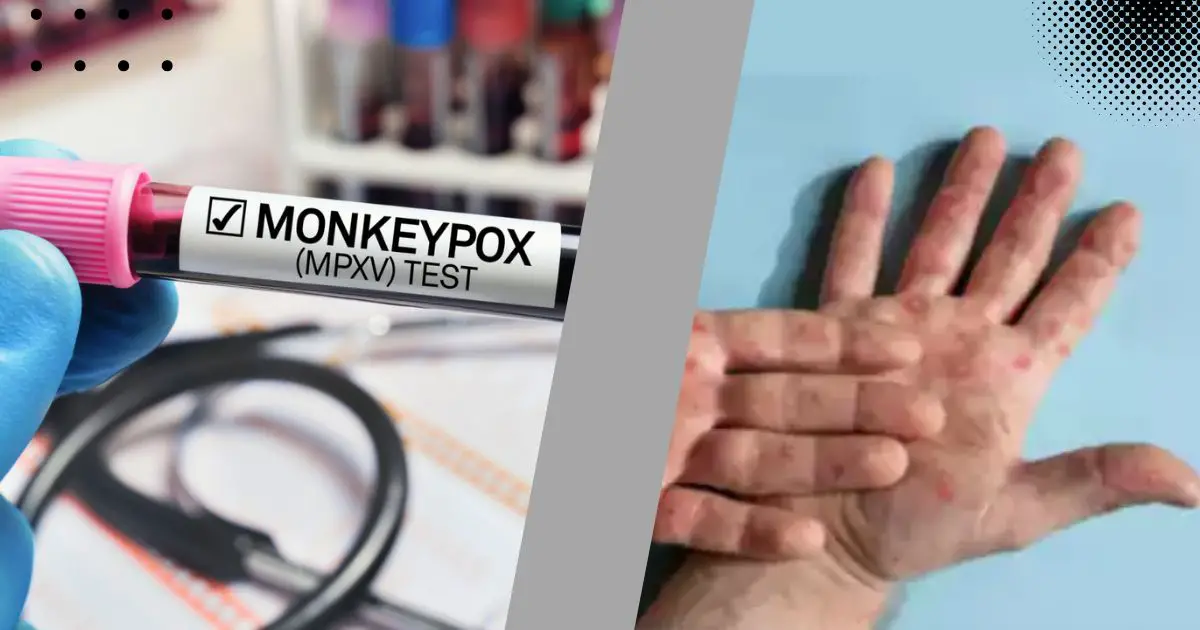
Mpox is a viral zoonotic disease caused by the mpox virus, which is related to the variola virus that causes smallpox. It primarily affects rodents and other animals, but humans can become infected through direct contact with an infected animal or human.
Historical Context in India
While mpox may not be as widely recognized as other viral infections, India has reported cases sporadically, with a notable increase in awareness due to recent global outbreaks. The World Health Organization (WHO) classified mpox as a public health concern, prompting nations, including India, to monitor and manage potential outbreaks.
How Mpox Spreads
Understanding the transmission of mpox is vital to mitigating its spread. Unlike COVID-19, which is primarily airborne, mpox is transmitted through direct contact with the bodily fluids or lesions of an infected person or animal. The primary modes of transmission include:
Direct Contact: This is the most common method of transmission. Touching skin lesions or bodily fluids of an infected person can lead to infection. This includes contact during sexual activity, where lesions may be present.
Respiratory Droplets: While mpox is not classified as airborne, respiratory droplets can spread the virus through close face-to-face contact, particularly if the infected person has lesions in their throat or mouth. However, this mode of transmission is less common compared to direct contact.
Contaminated Objects: The virus can survive on surfaces and objects, such as bedding or clothing, that have been in contact with an infected person or animal. Handling these contaminated items can result in transmission.
Animal to Human: Infections can occur when a person comes into contact with the blood, bodily fluids, or lesions of an infected animal, particularly rodents or primates.
Who is at Risk?
Understanding who is at risk for mpox infection helps in targeted public health messaging and preventive measures. The following groups are particularly vulnerable:
1. Close Contacts of Infected Individuals
Individuals who have had close contact with someone diagnosed with mpox are at the highest risk. This includes family members, sexual partners, and healthcare workers who may come into contact with infected patients.
2. Healthcare Workers
Healthcare workers who are not following appropriate infection control protocols may be exposed to the virus, especially in settings where mpox cases are present.
3. Individuals Engaging in High-Risk Behaviors
People who engage in unprotected sexual practices or have multiple sexual partners are at a heightened risk of contracting mpox. The disease can be transmitted during intimate contact, particularly if lesions are present.
4. Travelers to Endemic Regions
Travelers visiting areas where mpox is endemic, especially in Africa, should be aware of the risks and take necessary precautions. The virus is endemic in several regions, and exposure to local wildlife increases the chance of infection.
5. Individuals with Compromised Immune Systems
Those with weakened immune systems, whether due to existing health conditions or medications that suppress immune function, are more susceptible to severe outcomes from mpox.
Prevention and Control Measures
Given that mpox spreads primarily through direct contact, several preventive measures can be employed:
1. Education and Awareness
Public education campaigns focusing on the nature of mpox, its transmission, and preventive measures are crucial. Awareness can empower individuals to recognize symptoms and seek prompt medical attention.
2. Safe Practices
Encouraging safe sexual practices, such as using condoms and having open discussions about sexual health, can help reduce transmission rates among high-risk populations.
3. Infection Control in Healthcare Settings
Healthcare facilities must implement strict infection control measures, including the use of personal protective equipment (PPE) when handling patients with suspected or confirmed mpox.
4. Surveillance and Reporting
Robust surveillance systems for tracking mpox cases can help contain outbreaks. Timely reporting of cases to public health authorities enables swift response measures.
5. Quarantine and Isolation
In the event of an outbreak, isolating infected individuals and quarantining those who have been in close contact can help prevent further spread of the virus.
Conclusion
Mpox is not a new concern for India, but it requires renewed attention and understanding in light of recent global health alerts. Unlike COVID-19, mpox does not spread through airborne transmission but rather through direct contact with infected individuals or animals. By recognizing the modes of transmission and identifying those at risk, public health initiatives can be more effectively tailored to combat this disease. Education, safe practices, and vigilant healthcare responses will be key in managing and mitigating the impact of mpox in India and beyond.